By MATTHEW HOLT
Today we’re going to have fun with show and tell. I’m going to show you how a little corner of American health care is making my life as a consumer worse and more expensive–hopefully someone can tell me why.
The cast members are: me, my MD, the (sort of) independent pharmacy that delivers, Alto, and my insurer Blue Shield of California and its PBM CVS Caremark, which also owns a mail order pharmacy.
The brief backstory: For some years my doctor has been whining about my high cholesterol, and a few years back I went on a statin called Rosuvastatin Calcium. Older readers may remember Jean Luc Picard himself advertising the branded version Crestor, but it’s been off patent for about a decade. About 50 million Americans now take a statin, almost all of them a generic, including many 60 year old males like me. My cholesterol has come down, but my MD told me it could come down more, so a few months ago we boosted the dose to 40mg from 20mg.
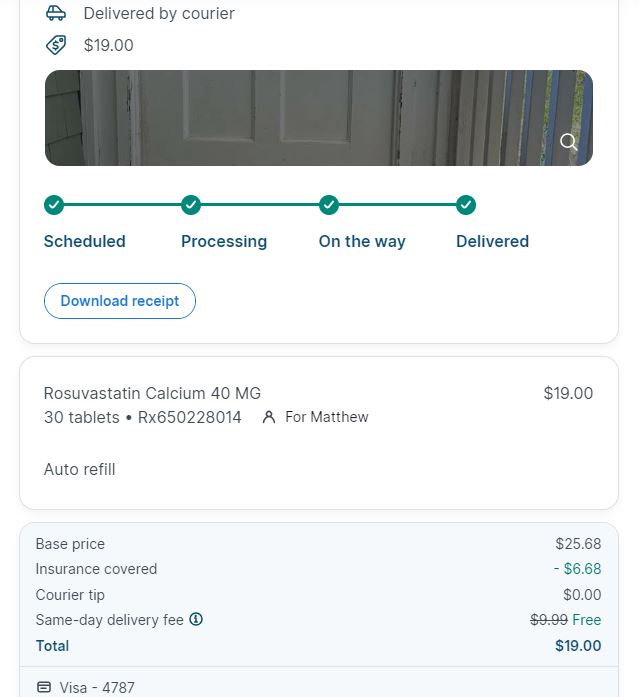
Until recently I’d been insured by BCBS Massachusetts, and you might recall a little over a year ago I wrote a piece on THCB about the fun and games to be had trying to figure out what their PBM (CVS Caremark) was doing with the pricing of my kid’s ADHD medication. But they’d never messed with my medication as my statins are cheap. At least I thought they were. In fact as recently as April last year, they were free. You can see the price from the delivery from Alto Pharmacy below.
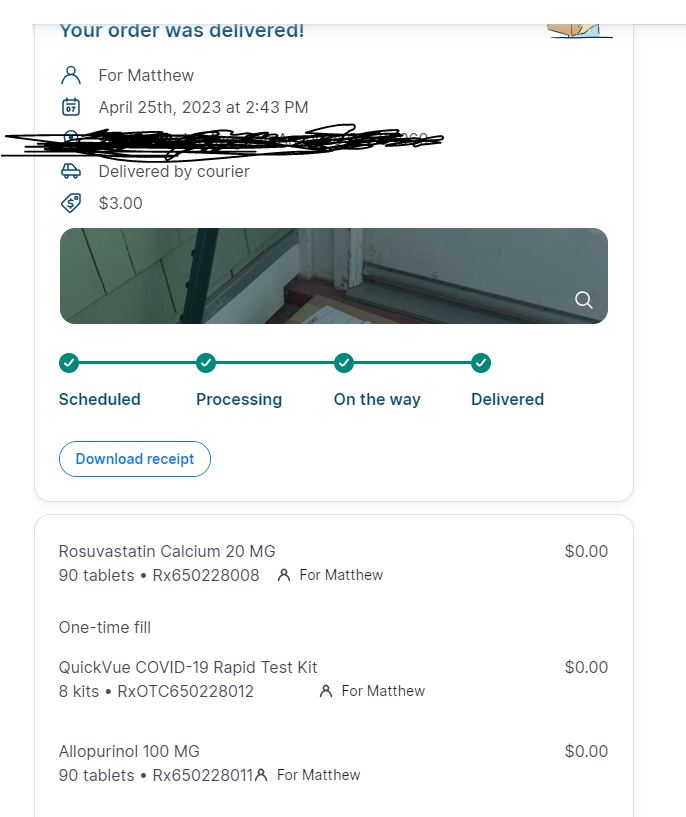
How BCBS Mass came up with $0.00 as the price I pay I don’t know, but presumably they think it’s a good thing to have me on statins in the hope I don’t have an (expensive) heart attack instead.
Then for some reason my price for the statin later the same year went up to $23. No longer $0 but at $8 a month not really worth making a fuss about.
At the end of the year, COBRA expired and I went to buy insurance on the California exchange. And in order to keep access to my family’s doctors at One Medical, I chose the only plan they were in, the Blue Shield of California HMO.
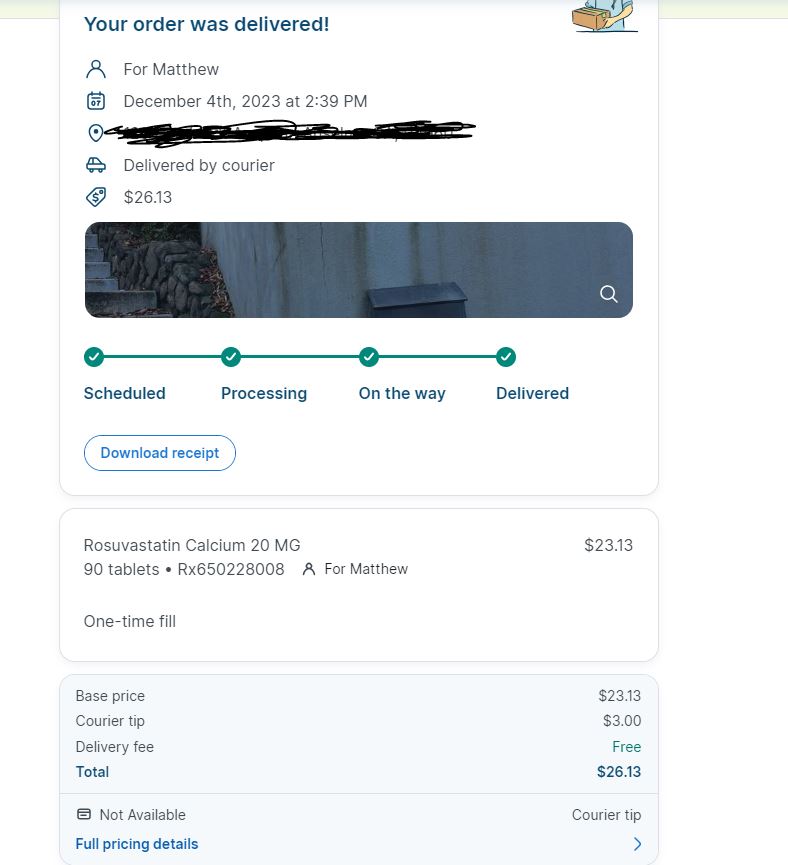
My next 90 day supply was the first one which went from 20mg to 40mg, but it’s still a common generic. Blue Shield of California also uses CVS Caremark (although it’s been talking a good game of ditching CVS Caremark and setting up its own PBM) and the cost at Alto barely budged. Now it was $28.
What happened next: So all was going normally until late last week when my next 90 supply was delivered. Except it wasn’t. Alto delivered me a 30 day supply and charged me $19.
Hang on, why change a 90 day supply for a med I am supposed to take every day forever for a 30 day one?
I enquire to Alto’s message system and they blamed Blue Shield.
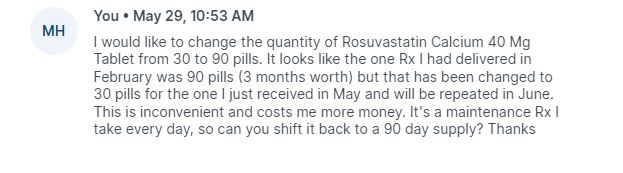
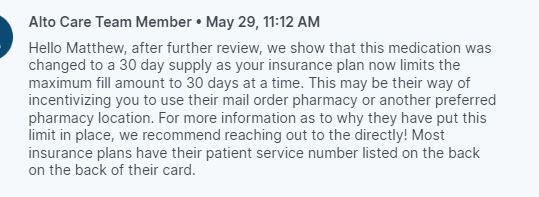
And of course Alto now is only allowed to fill my other meds on a 30 day cadence also.
So basically it looks like Blue Shield’s mail order service is playing hardball. They want me to move my 90 day order to them.
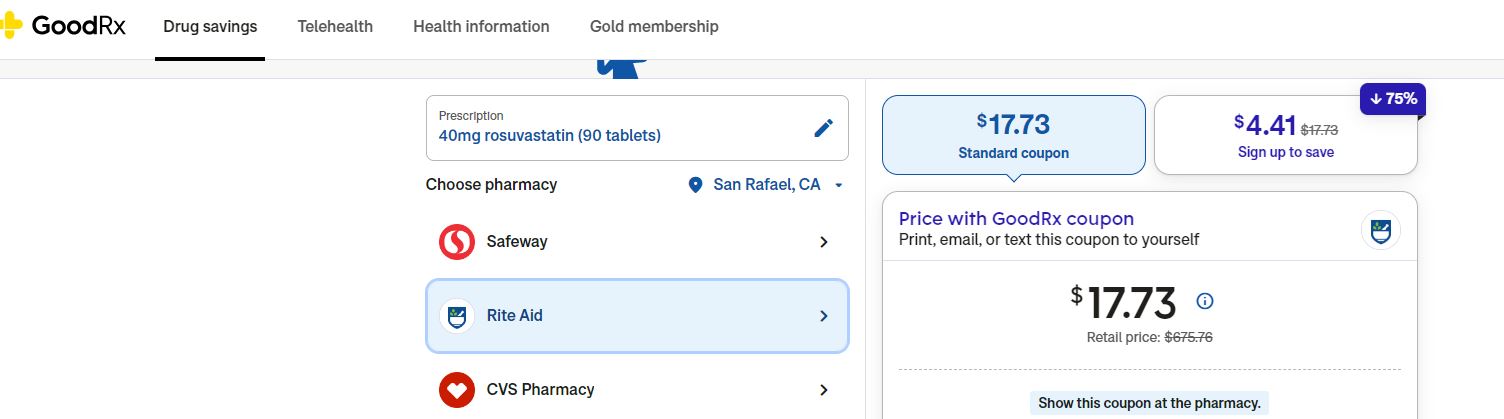
A diversion: Before I do that, it might be worth looking at what it costs for cash. GoodRx’s cheapest rate is about $18 for a 90 day supply. But of course I have to drive to pick it up, while Alto delivers. I’ll pay $10 more every 3 months for that.
Fun with customer service: So now to serve the good readers of THCB and because I am bloody minded about the consumer experience, I decide to find out from Blue Shield what is actually happening. (I also live tweeted the fun and games)
“I’m on with @BlueShieldCA hold music. Let’s see how they do in comparison with South Park….” (I’m sure you’ve seen the South Park version by now)
The answer is not well. BCBS Mass had a chat function, if no AI. Blue Shield of California has a phone line. With voice recognition that, well, doesn’t work.
After they ask me my date of birth and are convinced my sixty is a fifty. It’s also apparent their voice recognition cannot understand “NO” and yet they are so confident it’s perfect they won’t let me “Press 1 for yes or 2 for no”. But they’re happy to tell me that descriptions of benefits are not a guarantee of payment & I should schedule a wellness visit–even though they recognize my phone number and they’ve already paid for a wellness visit this calendar year. There’s over three minutes of irrelevant messaging, then 90 seconds of further identification which doesn’t work because it still can’t tell my birth year.
Blue Shield the tech leader: In its public pronouncements Blue Shield is claiming that it’s updating its tech. In fact Exec VP Peter Long has been boasting about it on Linkedin

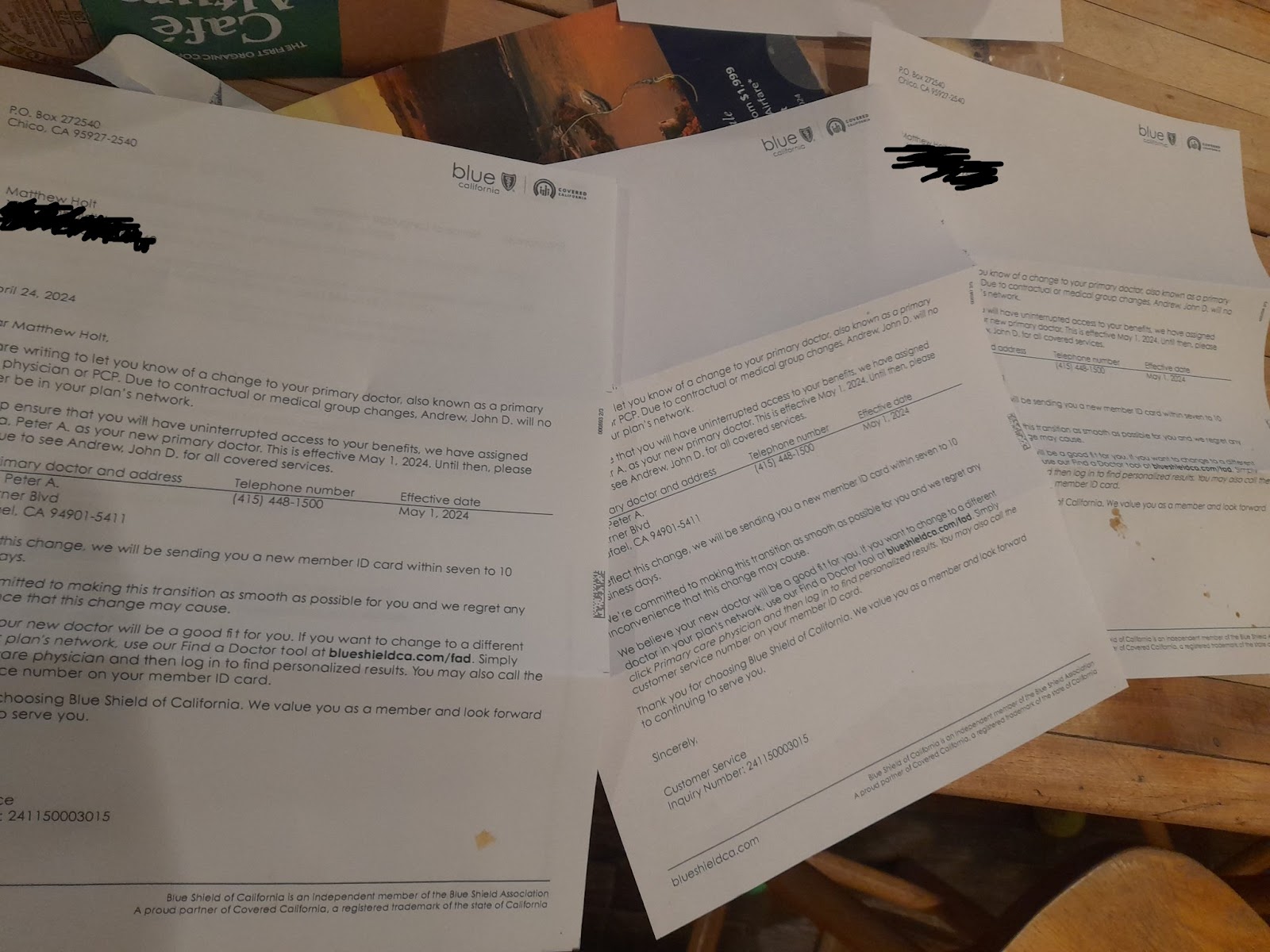
The regular tweet reader may recall them earlier this year sending me 5 identical letters to tell me that I had changed my PCP, which I had told them in the first place!
You may surmise that I’m not seeing their tech upgrades as improving my experience…yet.
So back to my statin. You’ll recall that it seems Blue Shield converted a maintenance statin I had been receiving from Alto Pharmacy to 30 days without telling me, and without allowing Alto to fill it for 90 days. Presumably they want to move this to their PBM/pharmacy to keep the profit.
My cost for 90 days was $28, for 30 days $19. So if I kept it with Alto my annual cost would go from around $112 to $228. So if I did nothing someone would be keeping the extra $116.
You may recall that I was on hold. An agent came on the line eventually and told me I have to speak to the pharmacy. After being on the call for 22 mins, someone came on and their opening words were to tell me that Blue Shield, “not us”, insists that I get this drug via mail order. So who are “you” I ask?“CVS Caremark” they say. So “how do I get my Rx via CVS Caremark” I ask? You can do it on the Blue Shield site. And if you hunt around a bit you can.
So I gamely click thru on the Blue Shield site, through to the CVS Caremark sub-site for Blue Shield, register with my ID number on the CVS Caremark site and get this:
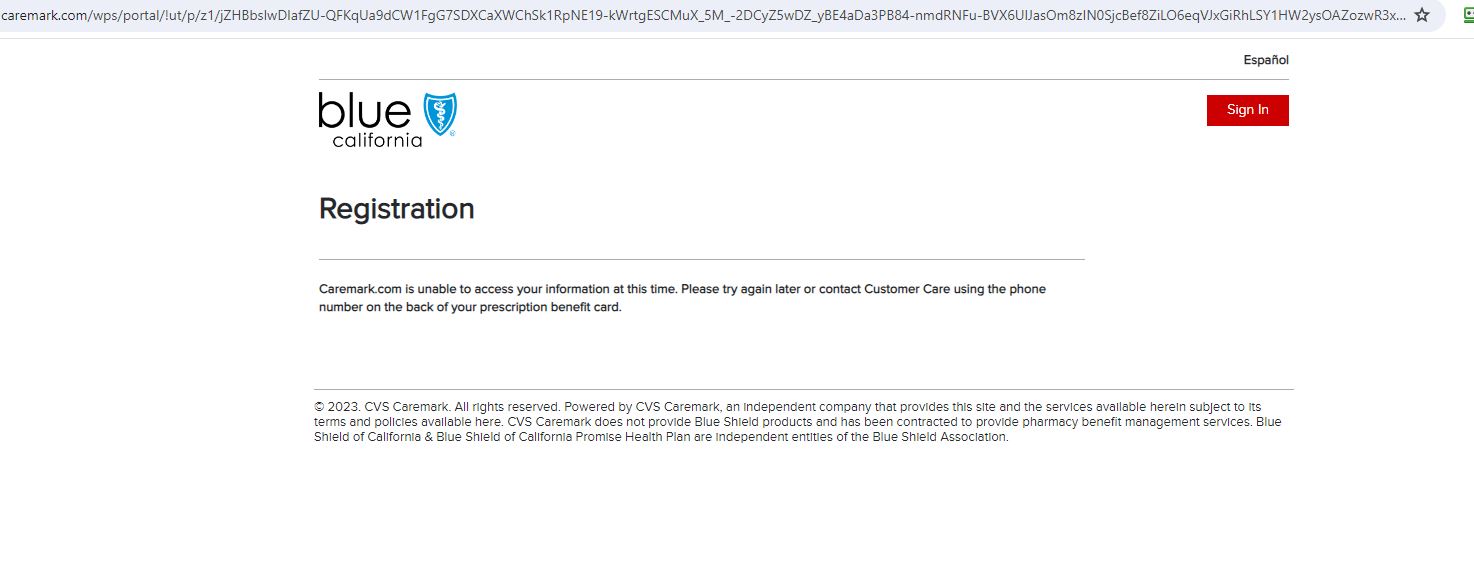
This has taken me 26 mins on the call, (not counting the first 5 min call that dropped), 10 mins screwing around on the @blueshield & @CVSHealth site, and of course the two sites can’t communicate…and they invite me to call back.
But because I am a sucker for punishment I try again, and see if I can figure some other way in the Blue Shield site. There I find a drug pricing tool.
I would like to know the cost to me of moving to the CVS Mail order. The tool knows the drugs I am on! I ask it for the price of my statin and it tells me it’s $19 for 30 days supply–the every price Alto charged me. It also tells me I can get 90 days via mail order!
So I click on that link and now it sends me to @cvspharmacy (again) , which lets me click on a recent Rx I have filled (I assume based on the claim from February) to see what the pricing is via mail order.
And of course you can guess what the response is.
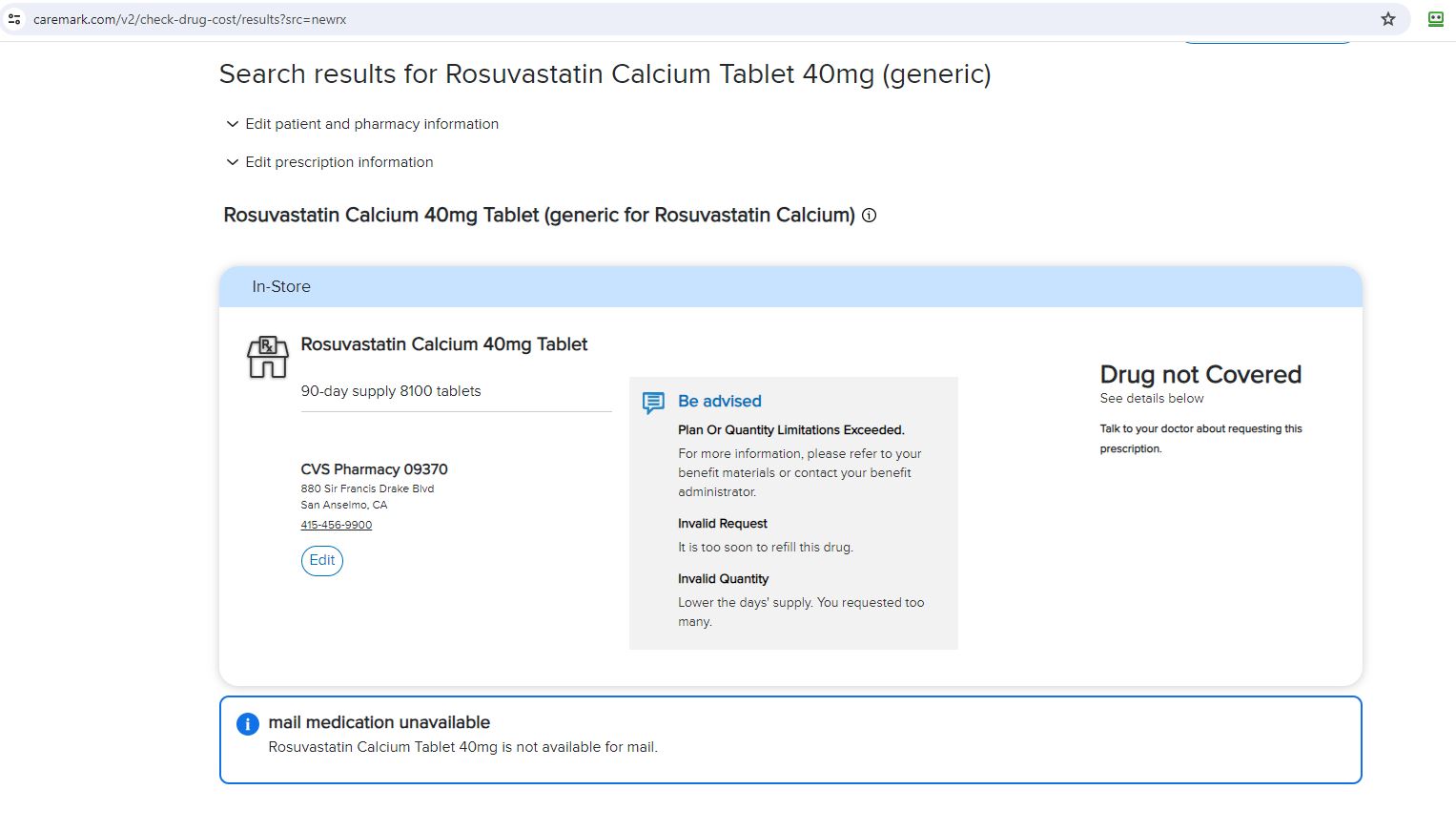
The answer is that 90 days supply is not available in a store and apparently neither is 90 days supply available via mail order. And for this fabulous experience they want to stop me using Alto Pharmacy. Presumably they want me to force my doctor’s office to resubmit the Rx to CVS mail order.
If you are still keeping score, somewhere between Blue Shield and CVS Caremark, for a maintenance drug that they want to encourage me to be on (I assume), which costs them almost nothing to acquire, they want me to change pharmacy and/or bother my doctor.
We still won’t know if it works, and for that matter it’s unsure who gets the extra $116 if I go back to 30 days at Alto.
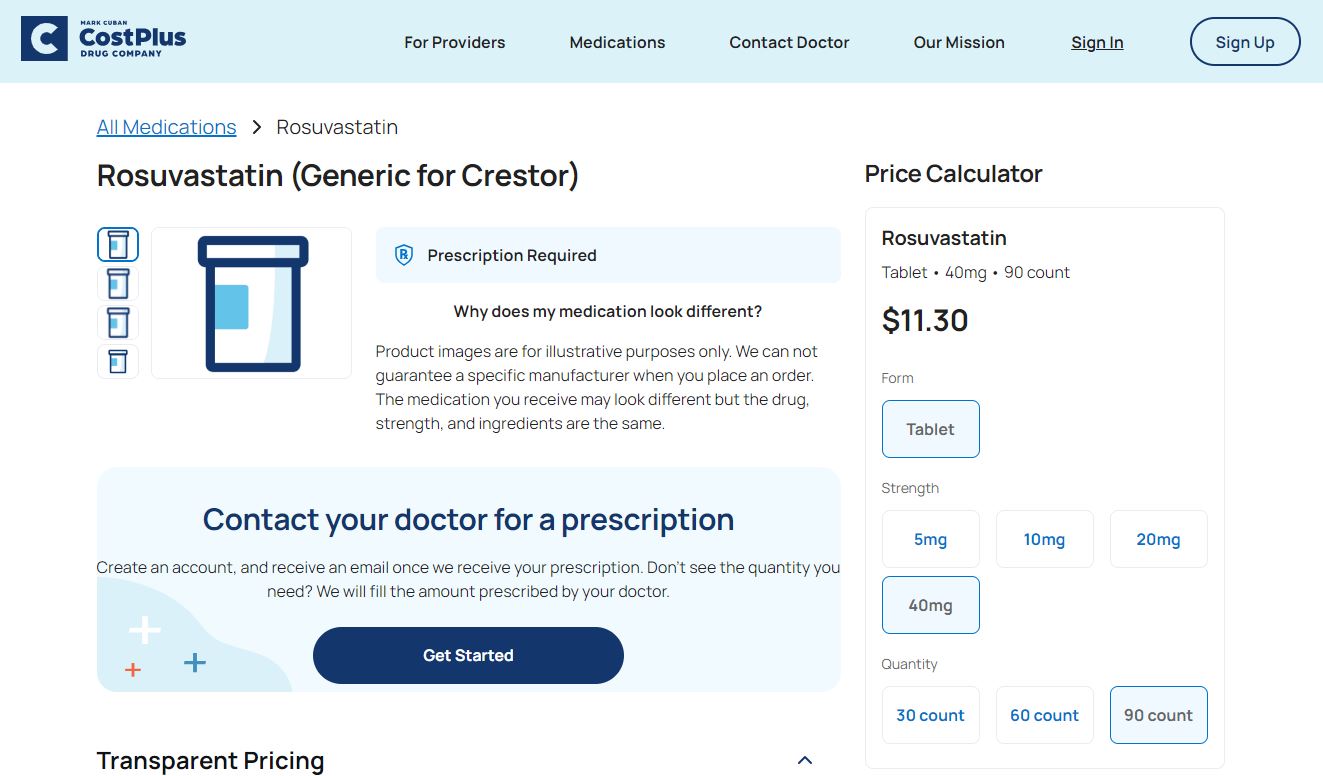
And of course it would be easier and cheaper for me to pay the $11 + shipping it would cost me to buy 90 days supply at Mark Cuban’s Cost Plus drugs. But then it wouldn’t count against my deductible, and my insurer, who presumably is supposed to care about my health and my Rx adherence, won’t know what drugs I am on.
I hope you’ve enjoyed this little journey through this obscure corner of the American health care system. Bonus points if you can explain why anyone would want to go through this, or what the hell Blue Shield or CVS Caremark are gaining for making me do it.