By MIKE MAGEE
If you talk to consultants about AI in Medicine, it’s full speed ahead. GenAI assistants, “upskilling” the work force, reshaping customer service, new roles supported by reallocation of budgets, and always with one eye on “the dark side.”
But one area that has been relatively silent is surgery. What’s happening there? In June, 2023, the American College of Surgeons (ACS) weighed in with a report that largely stated the obvious. They wrote, “The daily barrage of news stories about artificial intelligence (AI) shows that this disruptive technology is here to stay and on the verge of revolutionizing surgical care.”
Their summary self-analysis was cautious, stating: “By highlighting tools, monitoring operations, and sending alerts, AI-based surgical systems can map out an approach to each patient’s surgical needs and guide and streamline surgical procedures. AI is particularly effective in laparoscopic and robotic surgery, where a video screen can display information or guidance from AI during the operation.”
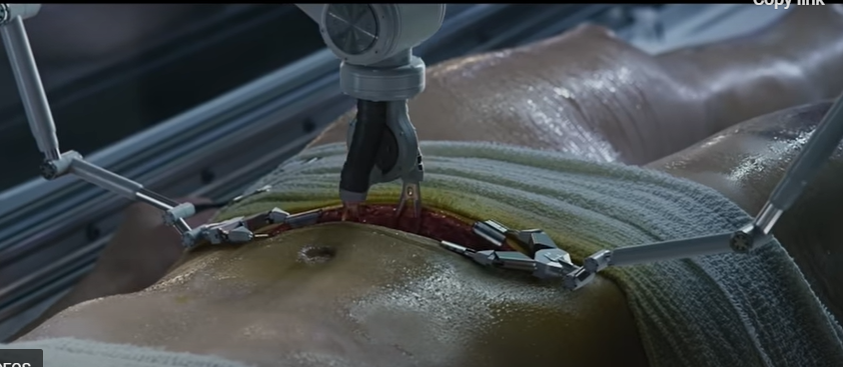
So the ACS is not anticipating an invasion of robots. In many ways, this is understandable. The operating theater does not reward hyperbole or flash performances. In an environment where risk is palpable, and simple tremors at the wrong time, and in the wrong place, can be deadly, surgical players are well-rehearsed and trained to remain calm, conservative, and alert members of the “surgical team.”
Johnson & Johnson’s AI surgery arm, MedTech, brands surgeons as “high-performance athletes” who are continuous trainers and learners…but also time-constrained “busy surgeons.” The heads of their AI business unit say that they want “to make healthcare smarter, less invasive, more personalized and more connected.” As a business unit, they decided to focus heavily of surgical education. “By combining a wealth of data stemming from surgical procedures and increasingly sophisticated AI technologies, we can transform the experience of patients, doctors and hospitals alike. . . When we use AI, it is always with a purpose.”
The surgical suite is no stranger to technology. Over the past few decades, lasers, laparoscopic equipment, microscopes, embedded imaging, all manner of alarms and alerts, and stretcher-side robotic work stations have become commonplace. It’s not like mAI is ACS’s first tech rodeo.
Mass General surgeon, Jennifer Eckoff, MD, sees the movement in broad strokes. “Not surprisingly, the technology’s biggest impact has been in the diagnostic specialties, such as radiology, pathology, and dermatology.” University of Kentucky surgeon, Danielle Walsh MD also chose to look at other departments. “AI is not intended to replace radiologists. – it is there to help them find a needle in a haystack.” But make no mistake, surgeons are aware that change is on the way. University of Minnesota surgeon, Christopher Tignanelli, MD’s, view is the future is now. He says, “AI will analyze surgeries as they’re being done and potentially provide decision support to surgeons as they’re operating.”
AI robotics as a challenger to their surgical roles, most believe, is pure science fiction. But as a companion and team member, most see the role of AI increasing, and increasing rapidly in the O.R. The greater the complexity, the more the need. As Mass General’s Eckoff says, “Simultaneously processing vast amounts of multimodal data, particularly imaging data, and incorporating diverse surgical expertise will be the number one benefit that AI brings to medicine. . . Based on its review of millions of surgical videos, AI has the ability to anticipate the next 15 to 30 seconds of an operation and provide additional oversight during the surgery.”
As the powerful profit center for most hospitals, dollars are likely to keep up with visioning as long as the “dark side of AI” is kept at bay. That includes “guidelines and guardrails” as outlined by new, rapidly forming elite academic AI collaboratives, like the Coalition for Health AI. Quality control, acceptance of liability and personal responsibility, patient confidence and trust, are all prerequisite. But the rewards, in the form of diagnostics, real-time safety feedback, precision and tremor-less technique, speed and efficient execution, and improved outcomes likely will more than make up for the investment in time, training, and dollars.
Mike Magee MD is a Medical Historian and regular contributor to THCB. He is the author of CODE BLUE: Inside the Medical Industrial Complex (Grove/2020)






